Introducing Fortuna Health - Revolutionizing Medicaid Enrollment
In a world where technology is transforming industries at an unprecedented pace, one startup is on a mission to simplify the complex process of Medicaid enrollment. Fortuna Health, founded in 2023 and headquartered in the bustling city of New York, has set out to become the "TurboTax for Medicaid." With a team of three dedicated founders, each bringing a unique set of skills and experiences to the table, Fortuna Health is poised to make a significant impact on the healthcare landscape.
Who Are the Visionaries Behind Fortuna Health?
Let's start by getting to know the driving forces behind Fortuna Health:
Cydney Kim - A healthcare operator with an impressive track record, Cydney has worked with industry giants like Halo Dx, McKinsey, and Bridgewater. Her expertise in healthcare operations and strategy has been instrumental in shaping Fortuna's vision.
Nikita Singareddy - Nikita is the brains behind Fortuna's mission to simplify Medicaid enrollment. With a background that includes stints at Truepill, a16z, RRE Ventures, and Oscar Health, she brings a wealth of knowledge from the healthcare and technology sectors.
Ben Wesner - As the first software engineer at Juniper (YC W21) and with previous experiences at Bloomberg and a Brown University graduate, Ben's technical prowess is a cornerstone of Fortuna's platform.
Fortuna Health - Revolutionizing Medicaid Enrollment with the TurboTax Approach
When it comes to simplifying the complex and often daunting process of Medicaid application filing and renewals, Fortuna Health stands out as a pioneering force, often likened to the revered TurboTax software for taxes. But what does this comparison entail, and why is it so significant in the realm of healthcare? To truly appreciate the innovation Fortuna Health brings to the table, we must delve deeper into the essence of their flagship product and its profound impact on Medicaid enrollment.
Imagine a world where applying for and renewing Medicaid coverage is as straightforward and user-friendly as filing your taxes with the click of a button. That's precisely the vision that Fortuna Health is striving to turn into reality. Medicaid, a vital healthcare lifeline for millions of Americans, has long been plagued by a labyrinthine bureaucracy and cumbersome paperwork. This is where Fortuna Health emerges as a game-changer.
The Problem - Why Does Medicaid Enrollment Need a Fix?
Before delving into the solution Fortuna Health offers, it's crucial to understand the problem they are addressing. Currently, around 90 million Americans rely on Medicaid for their healthcare needs. However, this vast group faces numerous challenges when it comes to eligibility screenings and the (re)enrollment process. Consumers often find themselves navigating glitchy websites and grappling with extensive paper Medicaid forms, a process that can take hours.
The consequences of these challenges are significant. Procedural issues, such as form errors or missing notices in the mail, account for a staggering 75% of disenrollments. This not only leaves consumers without coverage but also results in severe downstream consequences. Medicaid health plans (MCOs) lose over $30 billion from churn, healthcare providers suffer $13 billion in lost patient revenue and uncompensated care, and states waste $8 billion on administrative costs.
Furthermore, a looming crisis is putting 15 million enrollees at risk of losing Medicaid coverage in the next 18 months, making Medicaid enrollment a pressing issue.
The Fortuna Health Solution - Simplifying Medicaid Enrollment
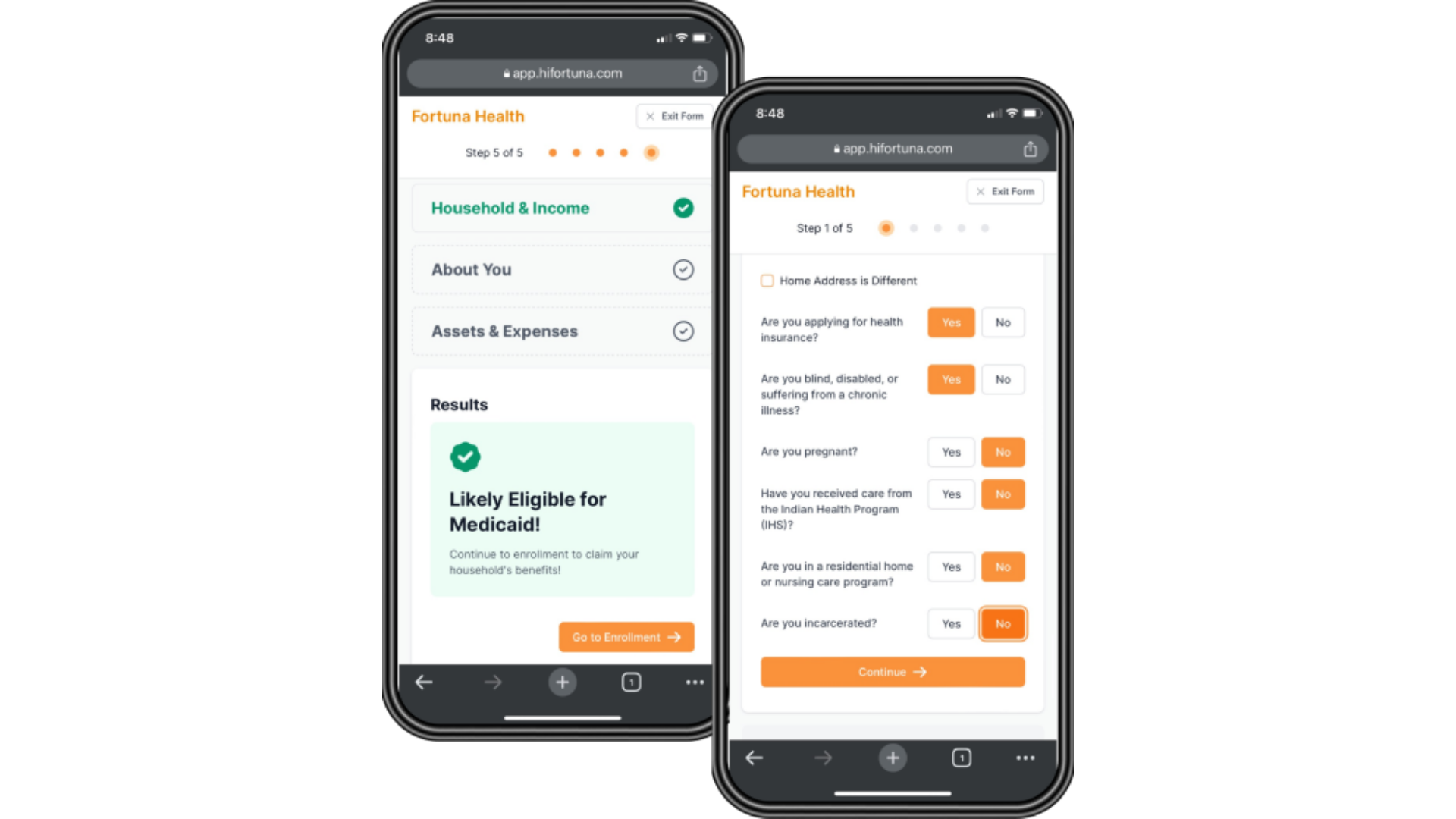
Fortuna Health is on a mission to solve the $57 billion enrollment problem with a consumer-centric approach. They've created a beautiful and simple web-based platform that offers a state Medicaid filing experience akin to using TurboTax for taxes. By focusing on creating products that consumers genuinely want to use, Fortuna Health has unlocked immense value for healthcare providers and health plans.
Here's what sets Fortuna's solution apart:
Seamless Web Experience: Fortuna offers consumers a seamless web experience, eliminating the need to interact with often cumbersome state portals.
Quick Eligibility Checks: They provide 60-second eligibility checks, ensuring consumers can quickly determine if they qualify for Medicaid.
Rapid (Re)Enrollment: Fortuna Health streamlines the (re)enrollment process, reducing it to just 5 minutes, and offers this service in seven languages to accommodate diverse populations.
Account Connections: To expedite the completion of applications, Fortuna allows consumers to connect their accounts, which auto-populate their filings.
Virtual Mailbox: They provide a "virtual" mailbox for state and health plan communications, making it easier for consumers to stay informed.
Text Notifications: Fortuna sends text notifications for urgent actions, ensuring consumers never miss important updates.
Empowering Providers and Health Plans with Real-Time Insights
Fortuna Health isn't just focused on simplifying the consumer experience. They also provide healthcare providers and health plans with a previously unavailable level of real-time visibility into enrollment and revenue risk. With the Fortuna platform, providers and health plans can seamlessly monitor Medicaid enrollment status, track consumer next steps, receive real-time updates on contact information, and benefit from comprehensive analytics.
This newfound insight empowers healthcare organizations to make informed decisions and streamline their operations in an industry where data-driven decisions can be a game-changer.
Fortuna Health's Vision - Transforming the Medicaid Ecosystem
Fortuna Health's vision extends far beyond their current offerings. They aim to transform the entire Medicaid enrollment experience and expand their product portfolio to become the consumer-facing digital infrastructure that powers the $800 billion+ Medicaid ecosystem.
By simplifying Medicaid enrollment and providing real-time insights, Fortuna Health aims to bring much-needed efficiency to an industry that impacts the lives of millions of Americans.
The Team - Experienced Operators and Engineers
Behind every successful startup is a dedicated team, and Fortuna Health is no exception. The founders bring a wealth of experience and expertise to the table, making them well-equipped to tackle the challenges of the healthcare industry.
Cydney, Ben, and Nikita all have backgrounds in scaling early and mid-stage healthcare startups. Cydney's experience as a General Manager and VP of Operations and Strategy at a health tech company with a significant Medicaid patient base is invaluable. Ben's technical acumen as the first software engineer at Juniper and Nikita's experience at Oscar Health and Truepill add a strong technological and healthcare foundation to the team.
Conclusion - Fortuna Health's Bold Mission
In conclusion, Fortuna Health is on a bold mission to revolutionize the Medicaid enrollment process. With a consumer-centric approach, a robust technical platform, and a team of experienced operators and engineers, they are well-positioned to make a meaningful impact in an industry ripe for innovation. As the "TurboTax for Medicaid," Fortuna Health is not only simplifying the lives of millions of Americans but also creating significant value for healthcare providers, health plans, and the states themselves. Keep an eye on this startup, as they work towards transforming the Medicaid ecosystem for the better.